|
Part of having a Well Balanced Body is recognizing the many facets of health, healing, and wellness. The choices we make can make a significant impact on, not only our health today, but the distant future. What we consciously or unconsciously choose to put in our body daily and how we take care of our body is what really matters.
At Well Balanced Body, we strive to make preventative wellness at the cornerstone of our facility. Yet, we are putting out fires within the neuromuscular skeletal system as well as the digestive, endocrine, immune systems etc. We want to bridge the gap between pain management and living your absolute best life possible. Not just free of pain, but in full health and vitality. We want to add more life to your years. So what does that even look like? Everyone's definition of health is different. That may be because we are all so different. But, it also is due to the fact that as laymans -- we can’t fully know what health and illness actually look like. In a lot of cases, we must start with our intuition -- telling us something isn’t right and we must listen to our bodies and move in that direction. Unfortunately, it is common for us to ignore those signals early on and it isn't until there is a life and death situation before we really listen. Even though the definition of health may look different for all of us, we also have to admit that we have to start with prevention at some point. Where to start? Listening to your body:
I hear often, “I just don’t have time.” If there is anyone who gets the concept of “not having time,” It’s me. Running a business, taking care of patients, building and guiding a staff, raising a toddler and a little one, managing a household list of things to constantly do whilst striving for mental/emotional, spiritual, physical growth. There is no one that gets it more than I do. I have also suffered my deal of health heartbreaks -- but I realized where I went wrong. I allowed life to get the best of me. I got caught up in the “to dos” and also made those excuses. I am human. Which is why, more importantly, I am encouraging you to begin with breath. It’s the easiest way to tap into your nervous system. Most days, people hold their breath on the inhale. This is a stress response. So, to begin, we must lengthen our exhales. This is how you enter chill mode. Try this daily exercise, before bed, begin with 2 minutes, than add more throughout the day -- in the shower, driving, washing dishes, or maybe take a moment to close your eyes and breathe. Daily Breathing Exercise to Access The Chill Mode Of Your Nervous System
If you “don’t have time for breath.” Then you don’t have time for health. And if you are curious, the “chill mode” is the parasympathetic portion of the autonomic nervous system. This is where healing happens. The inhale is sympathetic, fight or flight, and the exhale is parasympathetic, rest and digest.
0 Comments
This Halloween you don't have to miss out on sweet treats! You can enjoy delicious treats without the harmful ingredients. Get into the spirit with some healthy treat alternatives! We've found these delicious Vegan Twix Bars from The Banana Diaries. And also these 3-ingredient Chocolate Crunch Donuts from Nadia's Healthy Kitchen. They don't take long to make and will be a fun treat for kids and adults alike!! Leave us a comment below if you decided to make them.
We like to make them in bar shape and cut them in thirds. Enjoy!! Happy Halloween! We continue to see devastating fire seasons over the past few years in California. They are also getting closer and closer to home.
Our hearts weigh heavy with all the stories and what families are having to go through. We can't even imagine. Your lungs + smoke Others who are further removed, like those of us in the Sacramento and surrounding areas, are experiencing symptoms like lung inflammation. In my work I’ve treated numerous firefighters, and have seen firsthand the effects that smoke has on their bodies, specifically the lungs. Many of our patients are coming in with lung inflammation and trouble breathing. Those inflicted with asthma are especially feeling the affects. Here are my top 5 tips to keep your lungs healthy: Get Adjusted By Your Chiropractor Positive clinical outcomes - increased chest expansion and oxygen rate post-adjustment - are seen in my office daily, not to mention the increased healthy immune system response that has been proven with Chiropractic adjustments. For even better results, see a Chiropractor who specializes in Applied Kinesiology. They are able to dive deeper into respiratory function, looking at diaphragmatic control and neuro-lymphatic drainage of the lung. Chiropractic also can address possible misalignment of cervical vertebrae which transmits nerve impulses to the diaphragm, which in turn, helps the diaphragm (your primary breathing muscle) function optimally. Eat Well Lung inflammation can also be linked to the consumption of inflammatory foods. The top 5 inflammatory foods to avoid in order of priority are:
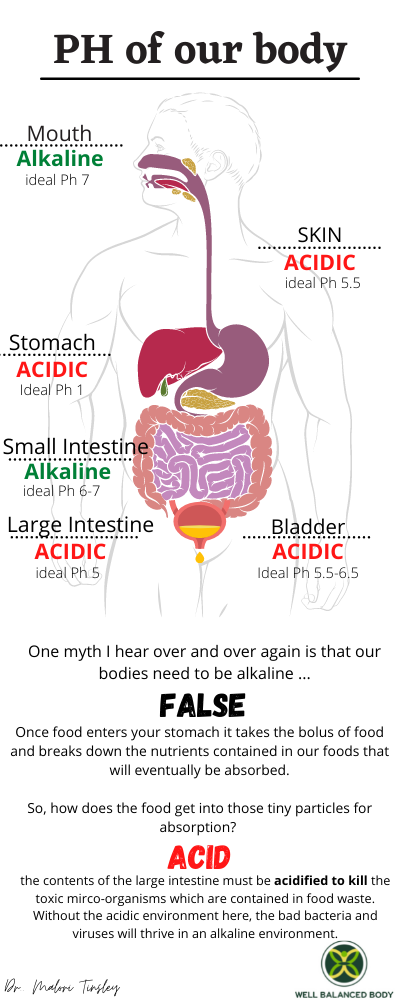
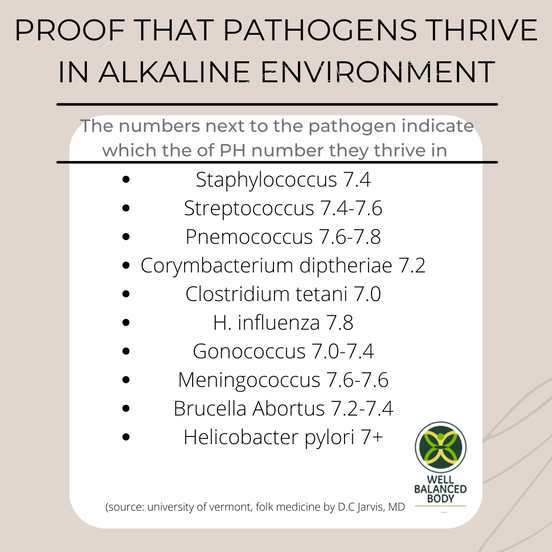
Need more specific recommendations - check out my healthy eating guide There are also a few things you can consume that help with lung function: 1.Vitamin e rich oils/fats: olive oil, grass fed butter, wheat germ oil. Please note: wheat germ does not contain gluten, so calm down! 2. Fatty fish- salmon, mackerel, sardines and anchovies. 3. Nuts and seeds (all raw organic). 4. Veggies. Lots of them! The main vegetables to be sure to include in your diet are garlic, onions and the cruciferous vegetables (broccoli, kale, collards, cabbage, cauliflower, watercress, etc). 5. Drink more water than usual. Recommended daily intake is half your body weight in ounces. I would add an extra 40 ounces to that with lemon and lime. Take Whole Food Supplements The Number One supplement I recommend to allow for better lung function is wheat germ oil. Cold processed wheat germ oil is a gluten-free concentrate made from the germ of the wheat kernel and provides the WHOLE vitamin E complex. Vitamin E is not just alpha tocopherol, which is ONLY the antioxidant or PROTECTOR of vitamin E complex. Vitamin E complex works together to support hormone precursors, support integrity of the tissues, and maximize oxygen levels. Wheat Germ Oil is the most concentrated, natural source of the complete vitamin E complex in the world. WGO is also a source of octacosanol, a nutrient that can increase your endurance and physical performance. which is good for vascular health, promotes cardiovascular health, prevents heart disease and age-related macular degeneration. I recommend taking this supplement to all my firefighter patients, anyone trying to increase muscular endurance, and to those who go to places of high altitude. Plus, people that have a personal or family history of cardiovascular health complications. WARNING: Do not consume synthetic OTC vitamin E - as it most likely ONLY contains the antioxidant portion of the vitamin E complex. Make sure you only consume whole food natural wheat germ oil. Diffuse essential oils My favorite oil blend to diffuse for lung health is Breathe by DoTerra. Lime and lemon are also great options to diffuse in your home. And last but not least… Workout INSIDE Check out a local yoga studio that will help you breathe better during class. Yoga teaches us specific breathing techniques that are always beneficial, but are especially so when we’re dealing with the effects of smoke in the air. ......................................................................................................... Two areas close to us that continue to be affected by fires year after year are El Dorado and Placer counties. There are two local nonprofits that we know support victims of the fires. Comment below if you know other local organizations that support our communities during these trying times. El Dorado Community Foundation (eldoradocf.org) Mosquito Fire Relief Fund | Placer Community Foundation (placercf.org) Stay Safe, Be Kind, and help where you can. Dr. T Hint: Our Bodies Are Mostly ACID! One myth I hear over and over again is that our bodies need to be alkaline - FALSE AND it actually sounds right, because acidic just sounds really bad, right? Well, I am going to shed some light on just how much our body needs to be acidic to thrive and function properly. Ok, let’s get started You are sitting down to eat your meal. Once food enters your stomach it takes the bolus of food and breaks down the nutrients contained in our foods that will eventually be absorbed. So, how does the food get into those tiny particles for absorption? ACID!!!!!! Our stomachs need to be a PH of 1-1.5, this is very acidic. The acid in our stomach is called hydrochloric acid. If you were to take this acid and drop it on your shoe, it would burn a hole in your shoe. That’s how acidic your stomach needs to be. The acidic environment of the stomach is not only useful for protein denaturing but also for protection against potentially infectious agents. Besides the mouth, this is the beginning part of your digestion. So, imagine, if your stomach was more alkaline………... The food would just sit in there and ferment, causing you to feel bloated, gassy, burpy, and even experience heartburn. Not to mention, without this vital acid in your stomach, your body wouldn’t be able to assimilate nutrients like protein, B12 and calcium from your foods. Eventually your lab work would indicate a deficiency. And you might experience symptoms of malnutrition. Such as fatigue, allergies, skin issues etc. Once the stomach breaks down protein it will dispel it into the small intestine - here the PH is actually very alkaline. The small intestine will further breakdown the protein into amino acids to pass easily through the walls of the small intestine and into the bloodstream to be utilized throughout the body. Remember, proteins are the building blocks of our body! After this, the contents of the intestine must be acidified again to kill the toxic mirco-organisms which are contained in food waste. Without the acidic environment here, the bad bacteria and viruses will thrive in an alkaline environment. The good bacteria in our guts are “acid loving” - hence the name ACIDophilus. Acidophilus (a probiotic) translates to acid-loving! We are acid loving beings!!!!
I hope this basic outline helped you understand, a little bit, how our bodies need to be mostly acidic. There is more deep diving we can do here into the subject, just how much how body relies on the Ph being more acidic. For now here are some things I will leave you with that will start to help balance out your bodies PH Things that you can do to help balance out the PH for better digestion
So as you can see we are mostly acidic beings! And I haven’t even touched on the skin and yes that is acidic as well! Simple Tests I recommend to determine if you PH is balanced
To balance out the body's PH, especially if you have a health concern related to the abnormal PH, I always recommend getting a qualified health care professional to discuss your lab findings and get you on the correct treatment plan. Remember, when your body is in balance, you are able to fight disease AND thrive to your fullest potential. click here book an appointment Sleeping Problems? Treat your body like Pavlov’s dog. The law of repetition says that the more you do something repeatedly, it becomes a habit ingrained in our psyche. Create a sleep routine. Much like you would for a baby, when you create a night time routine for them and repeat it everyday - you are signaling their bodies that it’s time to sleep soon. Once the routine is habitual, their body responds and they go to sleep. These are some of the things I do everynight.1. Perform nightly stretches: Throughout the day our bodies hold tension in areas that we overused. For example, if you are one that sits in front of the computer all day your body has now formed to that seated position. So, it doesn’t feel comfortable laying flat to go to sleep. You have to encourage your body to unwind and relax. Especially if you experience tightness in your hips, shoulder or neck when you are sleeping. This will help you. If you need help discovering what stretches you should be doing specifically, join the pain free movement series. 2. Diffuse Essential Oils: A relaxing oil is lavender. You can even place some oil on your temples. 3. Turn your phone on sleep mode This will silence all incoming calls, text messages, or alerts. You can respond in the morning. It will be okay. This one is so important. If you have an iphone, go to your clock app and click bedtime. When you set your bedtime for a certain time, your phone will stop all notifications. You can deal with any “emergencies” life may throw your way in the morning. This step has helped me tremendously to disconnect and prepare my body for a magical night's sleep. 4. Download the insight timer in the app store and play gentle, meditative music when you are getting ready for bed. You can even use this app for guided meditations before bed. 5. Deep Breaths: Check out the most recent blog to see how to hack your nervous system with breath. Extra help with Herbs 1. Ashwagandha: known for it’s adaptogenic qualities. It helps the body adapt to daily stressors. So, you can imagine if stress is hindering your ability to gain quality sleep, this herb might help. Infact, a recent 2021 study⁷ on Ashwagandha showed promising results. 150 subjects who suffered from low sleep quality ingested 120mg of the herb. After 42 days, not only did sleep quality drastically improve but the subjects reported no side effects whatsoever 2. Valerian root:²,³,⁴ for those who feel that they need restorative sleep. Nighty Night Extra by traditional medicinals is my go-to tea that contains valerian root. I drink this along with magnesium every night. It has a very mild sedative effect. 3. Rehmannia: This herb is used in chinese medicine to treat disorders related to aging.⁸ Which has been used for night sweats as it is a cooling and anti-inflammatory herb. 4. Kava: Ah, the infamous “kava coma.” Kava is known for its anxiolytic and sleep inducing effects⁹, hence the “coma”. I don’t often prescribe kava unless someone is desperate and desires to reach that coma-like state. One wellness patient of mine announced abruptly at her appointment that she was experiencing sleepless nights that were really frustrating her. I discussed her options based on her needs etc, once she heard “kava coma” come out of my mouth - she was ecstatic. The next day I received a message stating, “I slept, thank you. #kavacoma” So, what’s the deal with the kava coma?? Kava is not only helpful for inducing sleep related to anxiety. It also helps with relaxing the muscular system as well.¹⁰ Acting directly on inhibiting muscular contraction to induce relaxation. A very helpful herb for those who also experience muscle spasms. Kava works when the mind and body won't shut off. 5. California poppy: this herb is helpful for nerve pain related to insomnia; neuralgia, sciatica, and toothache.¹ 6. Skull cap: for the mind that won’t shut off. In numerous studies, we are understanding the benefits of this herb (along with rhodiola and lion's mane) as the same mind-relaxing benefits as an antidepressant. The bioactive ingredients found within S. baicalensis, H. erinaceus and R. rosea target the main biochemical events which are implicated in psychiatric conditions. mimicking at some extent the mechanisms of action of conventional antidepressants and mood stabilizers in the absence of serious adverse effects⁶ This is phenomenal information! You guys, not only do these herbs work on inhibiting the SAME neurological pathway that causes depression and anxiety -- they also work to “counteract oxidative stress, mitochondrial dysfunction, and inflammation” and without the crazy side effects. So they help with anxiety and depression while also combating toxic stress on the body!!! Are you having a mind-gasm yet?!In addition to aiding in mood, each herb in the study also has additional individual health benefits. “Including antitumor, hepatoprotective, antimicrobial, anti-inflammatory, anti-hyperlipidemic, antidiabetic, cardio-protective, neurotrophic,and neuroprotective effects”⁶ So basically these herbs help a whole bunch of health conditions. And again, without side effects -- they all have a favorable safety profile S. baicalensis, H. erinaceus and R. rosea produce neuroprotective effects in models of Parkinson’s disease (PD), Alzheimer’s disease (AD),, Huntington disease (HD), hypoxia/hypo-perfusion/stroke, nerve and brain injury, glutamate-induced neurotoxicity, and epilepsy.⁶ Skullcap contains baicalin which specifically initiates dopamine release, which is why it helps in so many neurological disorders. Biaclin also helps with memory related dysfunctions which are associated with the neurotransmitter, GABA. This is why this component of skullcap also helps with anxiety, ADHD, and depression. Depending on your specific need, we can create a sleep tincture that would contain a blend of herbs to help with sleep! I never recommend someone go on synthetic melatonin, this is a hormone, and can disrupt your endocrine system and circadian rhythms Other Factors That May Be Hindering Sleep....1. Nocturnal Hypoglycemia: If your blood sugar drops too low - this is a stressor to the human body - and it will increase adrenaline and norepinephrine to wake you up. Remedy this by eating a handful of raw nuts before bed. This can be the reason for dreaded night sweat or hot flash. However, there are other reasons for nocturnal night sweats/hot flashes, one being the liver. In general, it’s good to check fasting blood sugar, HA1c, cortisol, and liver enzymes on your labs to see where your numbers are. 2. Restless Leg Syndrome: This is due to the sympathetic nervous system, the stress response on overdrive and you can’t shut off your body’s signal to fight or flee. So your legs are basically still “running” even though you are laying down. A couple things that help that are helpful
3. Liver inflammation: The time of night that you wake up says something about an organ that may be hindered. Not necessarily a pathological disease. The liver can get burdened by the plethora of functions the liver does. One of which is to filter the blood of poisonous substances. If you tend to wake up at the same time every night, specifically between 1-3am, this is the time when the liver (an organ) is heightened. And therefore if it’s inflamed or burdened, you may be having a bit of trouble trying to do the many tasks for your body. Therefore you may need to get a further functional medicine analysis of your liver. For now you can try some lovely liver friendly veggies to the diet; like beets, artichokes, asparagus, globe artichoke, cauliflower, broccoli, arugula, and bok choy. I hope this sleep blog helps suss out where your sleep trouble is stemming from. At the bare minimum, start with stretching, breathing, and turning your phone on sleep mode. If you still need extra help, book a functional medicine appointment to help get to the root cause of your sleepless nights. To buy herbs or magnesium, visit our online store. References:
|
|






 RSS Feed
RSS Feed